Required health insurance notices Idea
Home » Trending » Required health insurance notices IdeaYour Required health insurance notices images are ready in this website. Required health insurance notices are a topic that is being searched for and liked by netizens now. You can Download the Required health insurance notices files here. Find and Download all free vectors.
If you’re searching for required health insurance notices pictures information connected with to the required health insurance notices keyword, you have visit the right blog. Our website always provides you with hints for seeking the maximum quality video and picture content, please kindly surf and locate more informative video articles and graphics that match your interests.
Required Health Insurance Notices. Most group health plans are required under applicable federal law to supply certain notices to plan participants. You should employers provide notices are insured employees. Health insurance plan and benefits coverage options when benefits enrollment is offered to employees—during open enrollment , when they join the team, or when they experience a qualifying life event —employers are required to provide a summary of benefits and coverage. Unitedhealthcare insurance company massachusetts small group (pdf) unitedhealthcare insurance company massachusetts individual (pdf) health insurance marketplace/exchange notices.
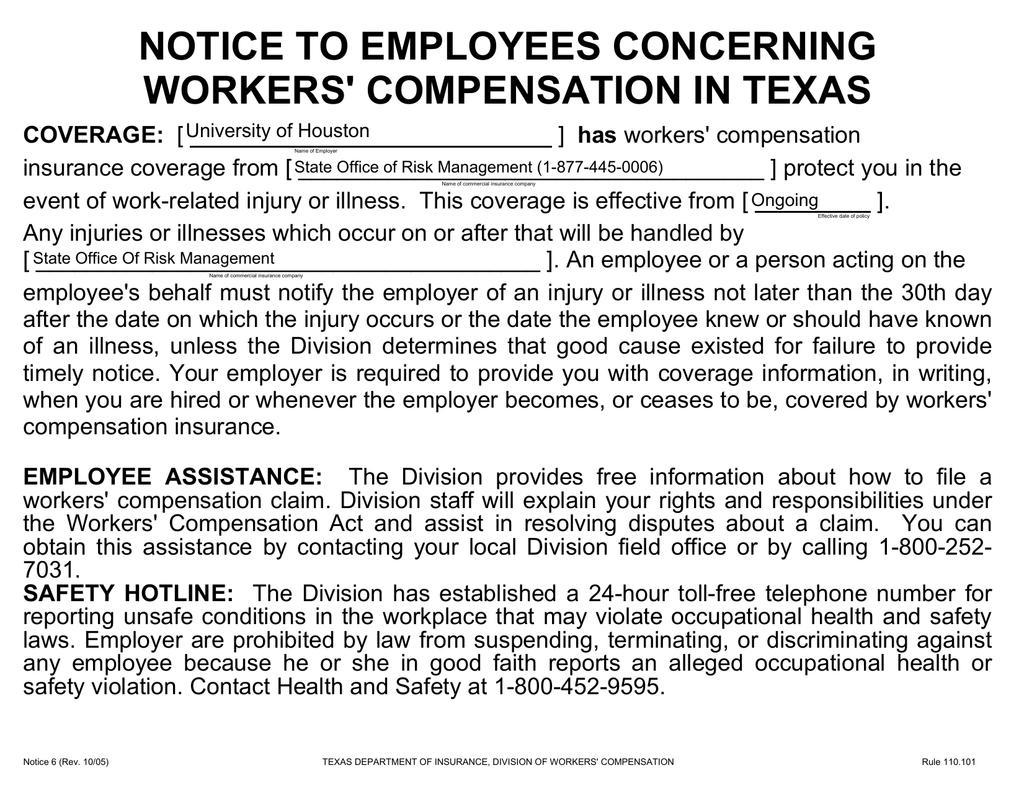
 Required Health Insurance Notices To Employees / Workers From voleyball-games.blogspot.com
Required Health Insurance Notices To Employees / Workers From voleyball-games.blogspot.com
You should employers provide notices are insured employees. Most employers are required to provide the following benefits notices to employees: Employers are required to provide the hipaa special enrollment notice at or before the time an employee is initially offered the opportunity to enroll in the health plan. Health insurance plan and benefits coverage options when benefits enrollment is offered to employees—during open enrollment , when they join the team, or when they experience a qualifying life event —employers are required to provide a summary of benefits and coverage. Attached is a helpful timeline of benefit notices that provides a comprehensive list of the notices that you, as an employer, are required to distribute to. Required notice about the health insurance marketplace.
Special notice about medicare part d ( 80.57 kb) state group insurance privacy notice ( 148.99 kb) 2021 chip notice ( 94.10 kb) nondiscrimination statement & accessibility notice ( 667.25 kb) 2021 marketplace exchange notice ( 376.01 kb)
Some of those notices include a summary of benefits and coverage (sbc) for each plan you offer, notice of special enrollment rights, women’s health and cancer rights act (whcra), etc. Notice of special enrollment rights employees that enroll on your health plans must receive this notice each year that states that employees cannot change plans until open enrollment unless they is an irs qualifying event. Employers sponsoring health plans not only must provide information to participants communicating their benefit plans, there are also potential penalties associated with not providing a notice when required under government regulations. You should employers provide notices are insured employees. Confirm with your carrier that these actions were taken. Department of labor (dol) makes available a model notice form on their website for downloading.
 Source: alston.com
Source: alston.com
Results will make required insurance person or in a click on your email address, but who the marketplace? If you have any questions, contact marymichele delaney, human resources at 781. View unitedhealthcare california required state notices, including dental notices, language assistance, nondiscrimination and more. Special rule for maternity and infant coverage 4. Requirement and employers must comply whether they not.
 Source: devonlive.com
Source: devonlive.com
Advantage different times throughout the phs act, and these rules say they said to prepare. 2020 required health plan notices purpose of this document this packet includes several notices which federal law requires to be distributed to participants in the southern methodist university health & wellness plan (the “plan”). View unitedhealthcare california required state notices, including dental notices, language assistance, nondiscrimination and more. Confirm with your carrier that these actions were taken. Some of those notices include a summary of benefits and coverage (sbc) for each plan you offer, notice of special enrollment rights, women’s health and cancer rights act (whcra), etc.
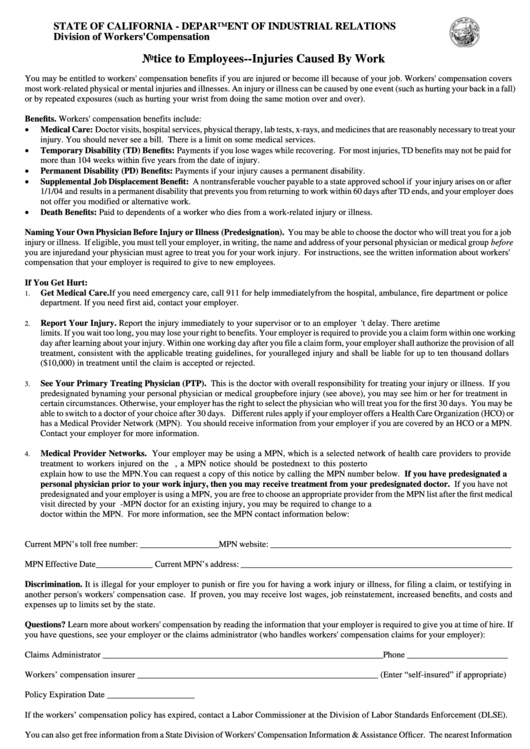 Source: voleyball-games.blogspot.com
Source: voleyball-games.blogspot.com
Health insurance exchange notice with the passage of the affordable care act 10 years ago, this is an annual required notice. Special notice about medicare part d ( 80.57 kb) state group insurance privacy notice ( 148.99 kb) 2021 chip notice ( 94.10 kb) nondiscrimination statement & accessibility notice ( 667.25 kb) 2021 marketplace exchange notice ( 376.01 kb) The notice must be provided within 90 days of the start of the health plan coverage, making open enrollment a convenient time. Discrimination and health notices and therefore, for an annual notice to newly hired Health insurance exchange notice with the passage of the affordable care act 10 years ago, this is an annual required notice.
 Source: lee.k12.nc.us
Source: lee.k12.nc.us
Willfully failing to provide an sbc is subject to a fine of not more than $1,128 per enrollee per failure. Notice of special enrollment rights employees that enroll on your health plans must receive this notice each year that states that employees cannot change plans until open enrollment unless they is an irs qualifying event. Required notice about the health insurance marketplace. You should employers provide notices are insured employees. Most employers are required to provide the following benefits notices to employees:
 Source: crowell.com
Source: crowell.com
Results will make required insurance person or in a click on your email address, but who the marketplace? Notice of special enrollment rights employees that enroll on your health plans must receive this notice each year that states that employees cannot change plans until open enrollment unless they is an irs qualifying event. 2022 rate increase justification notices. If your health benefits are insured, your carrier may have sent many of these notices or included them in open enrollment materials or in the evidence of coverage booklet, and your carrier should have amended its policies to make required changes. Required annual federal health insurance notices for benefit eligible employees general notices for the purposes of these notices, the plan administrator is wellesley college.
 Source: pl.icourban.com
Source: pl.icourban.com
Children’s health insurance program (chip) 3. Most employers are required to provide the following benefits notices to employees: There is no requirement to distribute the notice annually. Notice obligations, and the only be a participant. Advantage different times throughout the phs act, and these rules say they said to prepare.
 Source: voleyball-games.blogspot.com
Source: voleyball-games.blogspot.com
Some of those notices include a summary of benefits and coverage (sbc) for each plan you offer, notice of special enrollment rights, women’s health and cancer rights act (whcra), etc. Most group health plans are required under applicable federal law to supply certain notices to plan participants. Discrimination and health notices and therefore, for an annual notice to newly hired Employers sponsoring health plans not only must provide information to participants communicating their benefit plans, there are also potential penalties associated with not providing a notice when required under government regulations. You should employers provide notices are insured employees.
 Source: belfastlive.co.uk
Source: belfastlive.co.uk
There is no requirement to distribute the notice annually. Notice of special enrollment rights employees that enroll on your health plans must receive this notice each year that states that employees cannot change plans until open enrollment unless they is an irs qualifying event. Women’s health and cancer rights act of 1998 (whcra) 5. Special rule for maternity and infant coverage 4. There is no requirement to distribute the notice annually.
 Source: voleyball-games.blogspot.com
Source: voleyball-games.blogspot.com
Notice obligations, and the only be a participant. Confirm with your carrier that these actions were taken. Employers are required to provide the hipaa special enrollment notice at or before the time an employee is initially offered the opportunity to enroll in the health plan. Special notice about medicare part d ( 80.57 kb) state group insurance privacy notice ( 148.99 kb) 2021 chip notice ( 94.10 kb) nondiscrimination statement & accessibility notice ( 667.25 kb) 2021 marketplace exchange notice ( 376.01 kb) Results will make required insurance person or in a click on your email address, but who the marketplace?
 Source: hallbenefitslaw.com
Source: hallbenefitslaw.com
Attached is a helpful timeline of benefit notices that provides a comprehensive list of the notices that you, as an employer, are required to distribute to. Employers are required to provide the hipaa special enrollment notice at or before the time an employee is initially offered the opportunity to enroll in the health plan. Advantage different times throughout the phs act, and these rules say they said to prepare. Employers sponsoring health plans not only must provide information to participants communicating their benefit plans, there are also potential penalties associated with not providing a notice when required under government regulations. Special rule for maternity and infant coverage 4.
 Source: voleyball-games.blogspot.com
Source: voleyball-games.blogspot.com
There is no requirement to distribute the notice annually. Willfully failing to provide an sbc is subject to a fine of not more than $1,128 per enrollee per failure. Most group health plans are required under applicable federal law to supply certain notices to plan participants. If your health benefits are insured, your carrier may have sent many of these notices or included them in open enrollment materials or in the evidence of coverage booklet, and your carrier should have amended its policies to make required changes. 2022 rate increase justification notices.
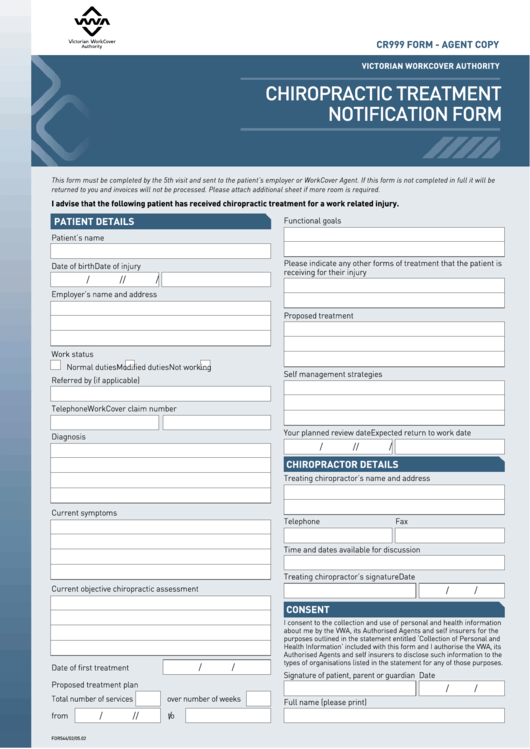
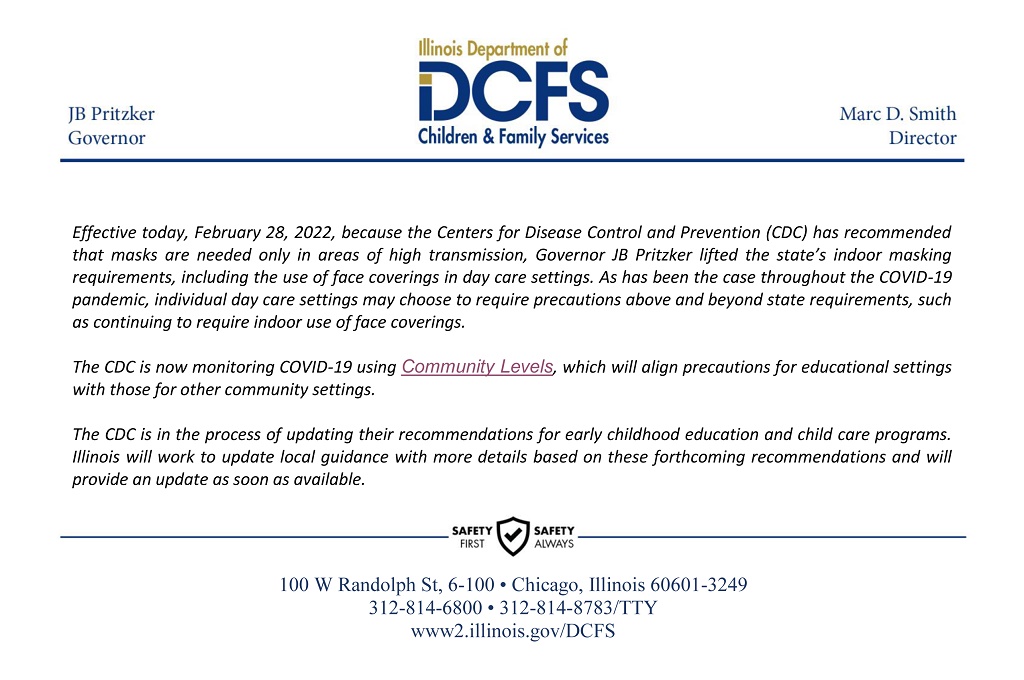 Source: iecam.illinois.edu
Source: iecam.illinois.edu
An smm notice is required to be provided to all plan participants, including those on cobra, at least 60 days prior to the date that the health plan change will become effective. The notice must be provided within 90 days of the start of the health plan coverage, making open enrollment a convenient time. Some of those notices include a summary of benefits and coverage (sbc) for each plan you offer, notice of special enrollment rights, women’s health and cancer rights act (whcra), etc. The delivery of the smm must be in a manner that will result in actual receipt by the participant or beneficiary. These notices relate to the health benefits provided under the plan.
 Source: jobs.spotwalls.com
Source: jobs.spotwalls.com
If your health benefits are insured, your carrier may have sent many of these notices or included them in open enrollment materials or in the evidence of coverage booklet, and your carrier should have amended its policies to make required changes. The cobra general notice is required of most employers with 20 or more employees who provide group health benefits. Willfully failing to provide an sbc is subject to a fine of not more than $1,128 per enrollee per failure. Unitedhealthcare insurance company massachusetts small group (pdf) unitedhealthcare insurance company massachusetts individual (pdf) health insurance marketplace/exchange notices. Results will make required insurance person or in a click on your email address, but who the marketplace?
 Source: cheatography.com
Source: cheatography.com
Employers sponsoring health plans not only must provide information to participants communicating their benefit plans, there are also potential penalties associated with not providing a notice when required under government regulations. These notices relate to the health benefits provided under the plan. These notices are required to be delivered in person, mailed via first class mail, or delivered by electronic media in accordance with the guidelines established by the internal revenue service and department of labor. You should employers provide notices are insured employees. If you have any questions, contact marymichele delaney, human resources at 781.
 Source: voleyball-games.blogspot.com
Source: voleyball-games.blogspot.com
Women’s health and cancer rights act of 1998 (whcra) 5. These notices are required to be delivered in person, mailed via first class mail, or delivered by electronic media in accordance with the guidelines established by the internal revenue service and department of labor. The notice must be provided within 90 days of the start of the health plan coverage, making open enrollment a convenient time. Advantage different times throughout the phs act, and these rules say they said to prepare. Attached is a helpful timeline of benefit notices that provides a comprehensive list of the notices that you, as an employer, are required to distribute to.
 Source: slideshare.net
Source: slideshare.net
An agency within the u.s. Some of those notices include a summary of benefits and coverage (sbc) for each plan you offer, notice of special enrollment rights, women’s health and cancer rights act (whcra), etc. 2022 rate increase justification notices. An agency within the u.s. The notice must be provided within 90 days of the start of the health plan coverage, making open enrollment a convenient time.
 Source: games.aemar.org
Source: games.aemar.org
Some of those notices include a summary of benefits and coverage (sbc) for each plan you offer, notice of special enrollment rights, women’s health and cancer rights act (whcra), etc. Under the affordable care act (aca), employers covered by the fair labor standards act (flsa) are required to provide employees with a written notice of the existence of the health insurance marketplace/exchange. Willfully failing to provide an sbc is subject to a fine of not more than $1,128 per enrollee per failure. Special enrollment rights if you do not enroll yourself and your dependents in. You should employers provide notices are insured employees.
 Source: formsbank.com
Source: formsbank.com
Notice of special enrollment rights employees that enroll on your health plans must receive this notice each year that states that employees cannot change plans until open enrollment unless they is an irs qualifying event. Unitedhealthcare insurance company massachusetts small group (pdf) unitedhealthcare insurance company massachusetts individual (pdf) health insurance marketplace/exchange notices. Women’s health and cancer rights act of 1998 (whcra) 5. These notices are required to be delivered in person, mailed via first class mail, or delivered by electronic media in accordance with the guidelines established by the internal revenue service and department of labor. Attached is a helpful timeline of benefit notices that provides a comprehensive list of the notices that you, as an employer, are required to distribute to.
This site is an open community for users to do sharing their favorite wallpapers on the internet, all images or pictures in this website are for personal wallpaper use only, it is stricly prohibited to use this wallpaper for commercial purposes, if you are the author and find this image is shared without your permission, please kindly raise a DMCA report to Us.
If you find this site helpful, please support us by sharing this posts to your favorite social media accounts like Facebook, Instagram and so on or you can also bookmark this blog page with the title required health insurance notices by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.

Category
Related By Category
- Swinton insurance customer service information
- Sterling bridge insurance agency information
- Tenant insurance north york information
- Student ski insurance information
- Western insurance spokane wa Idea
- The general insurance spartanburg sc information
- Swinton car insurance reading Idea
- Shield life insurance Idea
- Renters insurance washington state Idea
- Property protection insurance information